Calcium is important for the human as it helps in muscle contraction, nerve conduction, blood coagulation and release of enzymes & hormones. There are several regulatory mechanisms are there to keep blood calcium in the normal range, derangement of them can cause low or high Calcium in the blood.
What is hypercalcaemia?
Hypercalcaemia refers to high levels of calcium in the blood above the normal range (8.5-10.2 mg/dl).
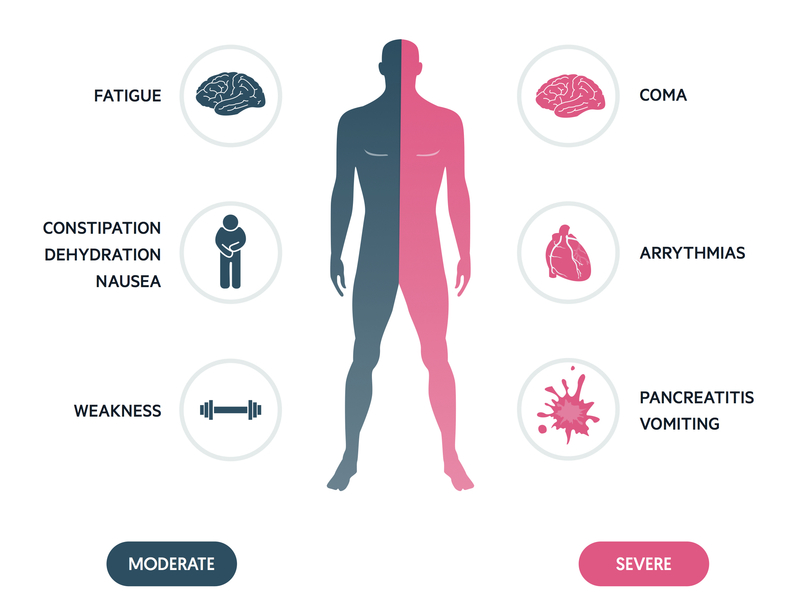
The symptoms can be diverse and depend on blood calcium levels
| Initial Nonspecific Symptoms | At Higher Calcium Levels |
|---|---|
| Excess urine & thirst | Abdominal pain |
| Loss of appetite | Vomiting |
| Depression | Dehydration |
| Muscle weakness | Lethargy |
| Nausea | Heart problem / coma |
| Constipation | Pancreatitis |
| Fatigue | Osteoporosis |
What are the causes of hypercalcaemia?
Primary hyperparathyroidism: Overactive parathyroid gland is the most common cause of hyperparathyroidism.
Other causes are
- Some types of tumours,
- Drugs- such as thiazide diuretics, excess vitamin D and vitamin A supplements
- Familial- e.g. familial hypocalciuric hypercalcaemia
What are the investigations required?
a. Fasting blood sample for:
- Total Calcium, Albumin, Phosphorous, Alkaline phosphatase
- PTH and Vitamin D levels
- Renal function tests
b. 24 hour urine calcium levels
c. In case of Primary Hyperparathyroidism a special scan of the parathyroid gland is required to localize the adenoma together with an assessment of bone mineral density
What are the treatment options available for high Calcium?
Medical management: Treatment for acute hypercalcaemia should be initiated in the hospital and will include
- Good hydration with saline
- Once circulating volume is normal, addition of diuretic e.g. furosemide
- Biphosphonates such as pamidronate and zoledronic acid or salmon calcitonin may be used to reduce bone turnover
- Plicamycin, gallium nitrate and prednisolone are also occasionally used.
- In severe cases haemodialysis may be effective
- Asymptomatic patients with PTH mediated hypercalcaemia which doesn’t meet the recognised criteria for surgery may be treated conservatively with regular monitoring of bone density, renal function and serum and urinary calcium levels
- Reduce patients intake of calcium
Surgical management: Surgical procedure will include removal of the affected gland or removing more than three glands in case all the glands are overactive.
Other Indications for Surgery
- 24 hr Urinary calcium excretion >400mg/day
- Bone density reduced at any site to a T score <-2.5
- Creatinine clearance (Kidney function) reduced by 30%
- Age >50years.
Treatment of the cause?
Once identified the cause of Hypercalcaemia, treatment should be directed to that a well. If overdose of vitamin D is the reason, it is easy, we need to withdraw the vitamin. More difficult, when it is due to malignancy, usually in most cases high calcium is a late feature and we can only offer palliative acre.
Are there any complications that can arise after surgery?
Transient, mild low calcium is common after surgery. In some cases, the low calcium may remain permanent when you need to be on Calcium and vitamin D treatment.
The hungry bone syndrome can develop if the overactive parathyroid was of some duration before surgery. This causes rapid influx of calcium into the bones causing more prolonged hypocalcaemia.
How to follow up post-operative cases?
Whatever the treatment or operation is done, we need life-long follow up regular intervals, sometimes maybe once a year.
Also see,