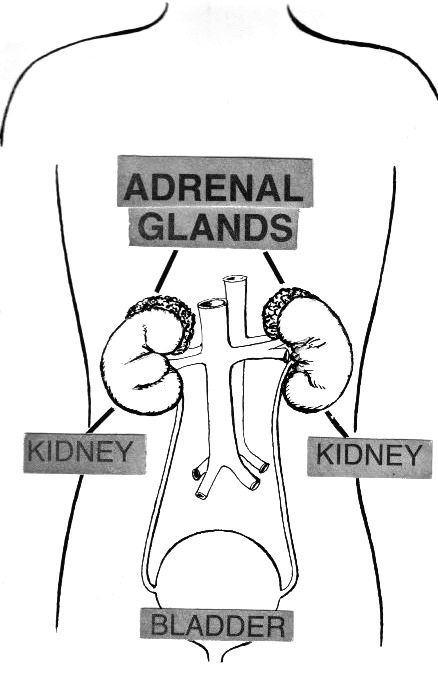
The adrenal glands are triangular shaped glands situated on top of the kidneys. Structurally each gland consists of a medulla (the center of the gland), which is surrounded by the cortex.
- Adrenal medulla – produces epinephrine and nor epinephrine (adrenaline)
- Adrenal cortex – produces cortisol (glucocorticoid), androgen and aldosterone
Both high and low Adrenal hormones can be life-saving, we need to recognise, investigate and treat them.
Underactive Adrenal or Hypocortisolism
What are the causes of Low cortisol hormone?
Low cortisol production is due to,
a. underactivity of adrenal gland (Addison’s disease or primary hypocortisolism)
- An infection like – tuberculosis,
- Autoimmunity.
- Tumour destruction.
b. Hypofunction of the pituitary (secondary hypocortisolism).
Addison’s disease occurs in all age groups and both sexes and is life-threatening, if not treated properly.
What are the clinical features of Addison’s disease?
Addison’s disease symptoms usually develop slowly, often over several months. Often, the disease progresses so slowly that symptoms are ignored until stress, such as illness or injury, occurs and makes symptoms worse.
Common presentations,
- loss of weight
- loss of appetite
- tiredness
- hyper-pigmentation of the skin
- dizziness and low BP
- nausea, vomiting,
- Abdominal pain
- Decreased axillary and pubic hair and reduced libido in women.
- Could be associated with vitiligo i.e. patchy whitening of the skin.
How do we confirm this?
- Blood investigations include
- Low blood sodium, High blood potassium, Low morning cortisol.
- Finding low blood cortisol, which fails to increase after injection of synacthen is diagnostic of Addison’s disease. This test is called short synacthen test.
- Protocol for Short synacthen test
- Fasting blood sample for Cortisol at 8 am
- Inj. Synacthen 250mg IM
- 30 mins later and 60 mins later blood for Cortisol.
- End of test
- Imaging: Computerized tomography (CT) scan of your abdomen to check the size of your adrenal glands and often with calcification. You may also undergo an MRI scan of your pituitary gland if testing indicates you might have secondary adrenal insufficiency
What is the treatment?
The treatment is reasonably simple, body is unable to give us the hormone, we will give it from outside. The most natural replacement is through tablet hydrocortisone, however prednisolone can also be used (cheap). The other hormone aldosterone is replaced by giving tablet fludrocortisone.
The initiation of hydrocortisone requires monitoring. This monitoring can be done by observing for several parameters like weight, BP, blood sodium and potassium levels, blood cortisol levels in the form of cortisol day curve
Another important thing to note is that this hydrocortisone tablet should be taken at a particular time of the day i.e. on waking, at midday and at 5 pm.
How to manage during an inter-current illness?
Cortisol is the hormone of fight and flight meaning to say that during any stressful event in a normal individual the level of the cortisol hormone goes up.
Trying to mimic what is normal, the requirement of cortisol goes up when a person with cortisol deficiency undergoes surgery or develops an illness.
The rule of thumb is to double the dose in illness like chest or urine infection. If unable to take tablet by mouth, you need to get an injection, this is a must otherwise you will develop a condition called Adrenocortical crisis.
Best is to keep an injection at home, in case of emergency can be used before getting in touch to Doctor.
Other treatment recommendations include:
- Carry a medical alert card and bracelet at all times
- Keep extra medication handy.
- Carry a glucocorticoid injection kit.
- Stay in contact with your doctor.
- Have annual checkups.
Also see,