Osteoporosis is a disease in which bones become fragile and more likely to break. If not prevented or if left untreated, osteoporosis can progress painlessly until a bone breaks. Osteoporosis per se is not the major illness, but it is the complications of the disease that are the major cause of concern.
Which are the bones most commonly prone for fractures?
These broken bones, also known as fractures, occur typically in the hip, spine, and wrist.
What are the various risk factors for developing osteoporosis?
| Modifiable risk factors | Nonmodifiable risk factors |
|---|---|
| Medications with negative effects on bone, like steroid | Being female |
| Sedentary – no weight bearing activity | Postmenopausal |
| Inadequate or excessive intake of nutrients | Small skeleton |
What happens to bone mineral density with age?
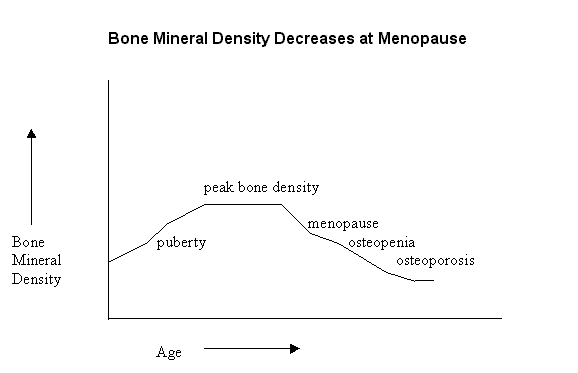
Bone mineral density increases until around age 25 and then levels off until age of 45-50yrs. During the first six to eight years of menopause, there is a sharp decline in bone mineral density in women.
The higher a woman’s overall bone density, the less she will be affected when she loses bone density at menopause. Men looses bone slowly after age of around 50 yrs.

What are the various investigations done to detect osteoporosis?
Bone mineral density using a DEXA (Dual energy X-Ray absorptiometry) scan will help us detect osteoporosis. It is safe, non-invasive and painless, and is the most reliable diagnostic tool used to check bone density throughout the body. DEXA measures bone density in the hip bone, hand bone and lumbar spine; areas susceptible to loss of bone density and fracture. The test does require not special preparation patient’s part.
There are some blood tests like bone markers available now which sometime helps in management.

Understanding the Results of Bone Mineral Density Tests: T-score and Z-score
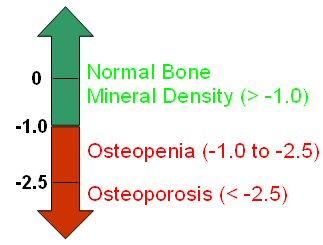
Bone mineral density (BMD) tests are performed to determine whether a patient has osteoporosis or osteopenia, a low bone mass that puts her at risk for osteoporosis.
To make this determination, the technologist will calculate the patient’s T-score. The World Health Organization (WHO) established the criteria for determining the T-score.
By determining a patient’s T-score, we can determine whether a woman has or is at risk for osteoporosis:
We can measure a person’s Z-score with a BMD test. The Z-score compares the patient’s BMD with somebody of the same age and sex.
The Z-score is not used to confirm a diagnosis of osteoporosis because a favorable BMD measurement (compared to the average BMD measurement for the patient’s age group) does not mean the patient is not at risk for osteoporosis.
What can be done to lower the risk of osteoporosis?
Two very important things: be physically active and take adequate calcium/vitamin D.
If a person picked the one thing that would have the greatest impact on his/her life and lower the risk for a number of late effects and common adult health problems, it would be to make a lifetime habit of being physically active.
Regular exercise, at least five times a week for about 30-45 minutes, makes a huge difference in the strength of our bones.
What are the various treatment options available for osteoporosis?
The various treatment options available are
1. Bisphosphonates – This group of drugs can inhibit bone breakdown, preserve bone mass, and even increase bone density, reducing the risk of fractures.
Side effects include nausea, abdominal pain, and the risk of an inflamed esophagus. Common preparation is once a week, to be taken in empty stomach with lots of water.
You are expected to keep upright for an hour. Preparations also available as once a day or once a month, usually once a week we prefer. Now injectable Bisphosphonates are available.
2. Raloxifene – This medication belongs to a class of drugs called selective estrogen receptor modulators. Raloxifene mimics estrogen’s beneficial effects on bone density in postmenopausal women, without some of the risks associated with estrogen, such as the increased risk of uterine cancer and, possibly, breast cancer. Hot flashes are a common side effect of Raloxifene.
3. Calcitonin – A hormone produced by thyroid gland, calcitonin reduces bone resorption and may slow bone loss. It may also prevent spine fractures, and may even provide some pain relief from compression fractures.
It’s usually administered as a nasal spray or by injection. Because calcitonin isn’t as potent as bisphosphonates, it’s normally reserved for people who can’t take other drugs. Injectable Calcitonin is helpful for pain related to spinal bone fracture.
4. Teriparatide – This powerful drug, an analogue of parathyroid hormone, treats osteoporosis in postmenopausal women and men who are at high risk of fractures. Teriparatide is given once a day by injection. It is well tolerated but little costly.
5. Strontium – Strontium is a mineral found along with calcium in most foods. Strontium supplements decrease bone resorption and also stimulate bone-building osteoblast activity and new bone formation in women with osteoporosis.
6. Denosumab is a human monoclonal antibody for the treatment of osteoporosis, a new medication was shown to reduce the risk of osteoporotic fracture in women and men.
Denosumab might be used in people who can’t take a bisphosphonate, such as some people with reduced kidney function. Denosumab is given subcutaneously under the skin every six months, usual adult dose Prolia 60 mg once every 6 months.
Adverse effects…common side effects are joint and muscle pain in the arms or legs, increased risk of infections such as cellulitis, hypocalcemia (low blood calcium), hypersensitivity allergy reactions and osteonecrosis of the jaw and atypical femur fractures.
Who should take Calcium supplements?
All people with an increased risk of osteoporosis should take Calcium supplementation.
Calcium supplementation is available in various forms. The RDA for calcium intake is based on the amount of elemental calcium in the supplement taken. The most commonly available is the Calcium carbonate; 500mg of this contains only 200mg of elemental Calcium.
Hence, at least 1gm of this is needed to give you approximately 400mg of elemental calcium.
There are other supplements which are available which contain vitamin D along with calcium. There are different types of vitamin D is available, it is better to confirm from your Doctor which would be best for you rather than buying over the counter.
While taking these supplements, a word of caution about the blood level of Calcium, as they tend to go up and cause other problems.
Also see,